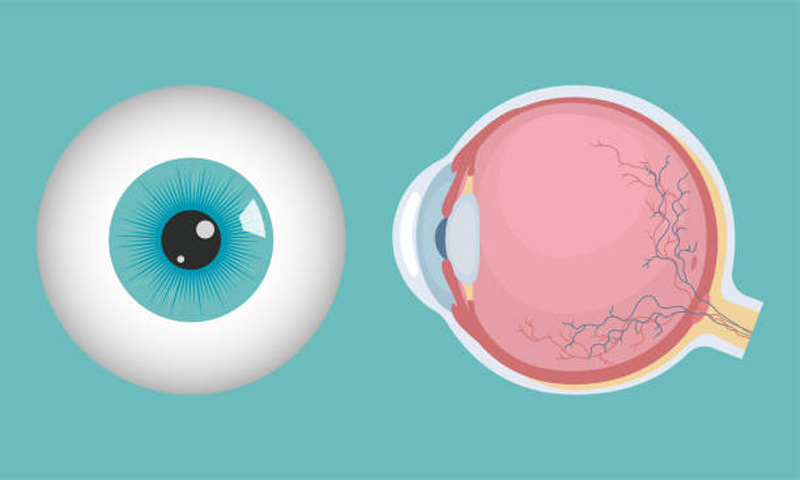
Diabetic retinopathy (DR) is a form of diabetes that affects the eyes and is commonly caused by damage to the patient’s blood vessels. The light-sensitive tissue sitting at the back of the eye or retina can be damaged, eventually resulting in blindness. Initially, diabetic retinopathy may not present any symptoms or may only exhibit mild vision issues. According to a Seattle eye doctor, the condition may develop in patients with type 1 or type 2 diabetes. If left untreated, the condition may result in blindness. Visit the Top Eye Doctors Near Me directory to find a list of top Seattle eye doctors.
People who’ve been diagnosed with diabetes have damaged blood vessels in their eyes due to high blood sugar. This alters their structure and function. Similarly, the vessels may thicken, close off, develop clots, leak, or grow microaneurysms. In most times, fluid accumulates in the retina, particularly the part used in performing tasks such as reading, a condition known as macular edema. In severe cases, the retina is deprived of its blood supply but instead grows new, defective vessels through a process known as neovascularization. The blood vessels in the eye are small, delicate and can bleed, possibly creating scar tissue, vision-impairing hemorrhages, and even separation of the patient’s retina from the eye (retinal detachment). Moreover, the new vessels may block fluid flow within the patient’s eye, resulting in glaucoma.
Causes, risk factors, and complication
One of the major causes of DR is the accumulation of sugar in the blood can block the tiny blood vessels that supply and nourish the retina, ending the blood supply. The eye then tries to grow new vessels but they don’t develop well and may leak easily. Anyone with diabetes is at risk of developing DR. Below are the risk factors for developing DR.
- Duration of diabetes, as having diabetes for extended periods of time can raise the risk of developing the condition
- High blood pressure
- Poor control of blood sugar level
- High cholesterol
- Tobacco use
- Pregnancy
- Being African-American/ Native American/ Hispanic
Complications may result in serious vision problems, including retinal detachment, glaucoma, vitreous hemorrhage, blindness, and glaucoma. Retinal detachment is when the scar tissue is detached from the retina located at the back of the eye. When this occurs, the patient may see spots floating in their vision. There may also be flashes of light in the vision or severe loss of vision. Glaucoma, on the other hand, occurs when new blood vessels grow in the front part of the patient’s eye, potentially causing a buildup of pressure inside of the eye. The pressure can cause damage to the optic nerve that relays images from the eye to the brain.
Vitreous hemorrhage occurs when the blood vessels bleed into the vitreous humor. Mild bleeding may lead to only a few floaters (dark spots). In extreme cases, blood fills the vitreous cavity and blocks your vision. Whereas vitreous hemorrhage may not cause permanent vision loss by itself, the damaged retina may make it difficult for your vision to return to its previous state of clarity. However, in most cases, the blood tends to clear from the eye in weeks or months. Eventually, the conditions can result in glaucoma or even total vision loss.
Testing and diagnosis
Anyone with diabetes should go for annual eye exams so that an ophthalmologist can help to detect diabetic retinopathy early before it advances to create further complications. An ophthalmologist will ask several questions about your medical history in addition to your vision history. You may also be asked to read an eye chart or get ready for examination of the retina using an ophthalmoscope. A basic eye exam may not detect some of the signs of diabetic retinopathy. The doctor may also have to administer drops to help dilate the pupil and have a better view of the retina using lenses and a slit lamp (a special light). The eye doctor may also administer fluorescein angiography to show changes to the retinal blood vessels in terms of structure and function.
Prevention
Retinal retinopathy can be prevented by going for regular eye exams and gaining control of your blood pressure and blood sugar. Early intervention can help to manage vision problems and prevent severe vision loss. Increased physical activity and a healthy diet can also help to manage diabetes. Doctors also recommend monitoring your blood sugar level, doing glycosylated hemoglobin tests, controlling your cholesterol and blood pressure, quitting smoking, and paying close attention to vision changes.
Treatment
Treatment depends on the type of DR, as it is aimed at slowing or stopping progression. Mild/moderate nonproliferative diabetic retinopathy is closely monitored to determine when you might require treatment. Controlling your blood sugar can slow the progression of DR. in contrast, proliferative diabetic retinopathy, advanced DR or macular edema, may require surgical treatment. Other treatment options include photocoagulation, laser treatment that can slow/stop leakage of blood or fluid in the eye. The eye doctor may also consider panretinal photocoagulation, vitrectomy, and medical injection.
Diabetic retinopathy may have fewer to no symptoms in its early stages. However, having diabetes and being African-American are some of the risk factors of DR. Treatment options vary depending on the stage of the condition, as the doctor may monitor and slow down the progression of the disease or consider more drastic treatment options such as laser treatment.
Comments
comments