Aldosterone is a steroid hormone produced by the zona glomerulosa of the adrenal cortex. It plays a crucial role in regulating blood pressure and electrolyte balance by promoting sodium retention and potassium excretion in the kidneys. This hormone is a key component of the renin-angiotensin-aldosterone system (RAAS), which is activated in response to low blood pressure or low sodium levels. Elevated aldosterone levels can lead to conditions such as primary aldosteronism, characterized by hypertension and hypokalemia. Additionally, aldosterone has been implicated in cardiovascular and renal diseases, particularly in patients with diabetes mellitus, due to its hypertrophic and fibrotic effects on the heart and blood vessels.
Aldosterone is a steroid hormone produced by the zona glomerulosa of the adrenal cortex. It plays a crucial role in regulating blood pressure and electrolyte balance by promoting sodium retention and potassium excretion in the kidneys. This hormone is a key component of the renin-angiotensin-aldosterone system (RAAS), which is activated in response to low blood pressure or low sodium levels. Elevated aldosterone levels can lead to conditions such as primary aldosteronism, characterized by hypertension and hypokalemia. Additionally, aldosterone has been implicated in cardiovascular and renal diseases, particularly in patients with diabetes mellitus, due to its hypertrophic and fibrotic effects on the heart and blood vessels.
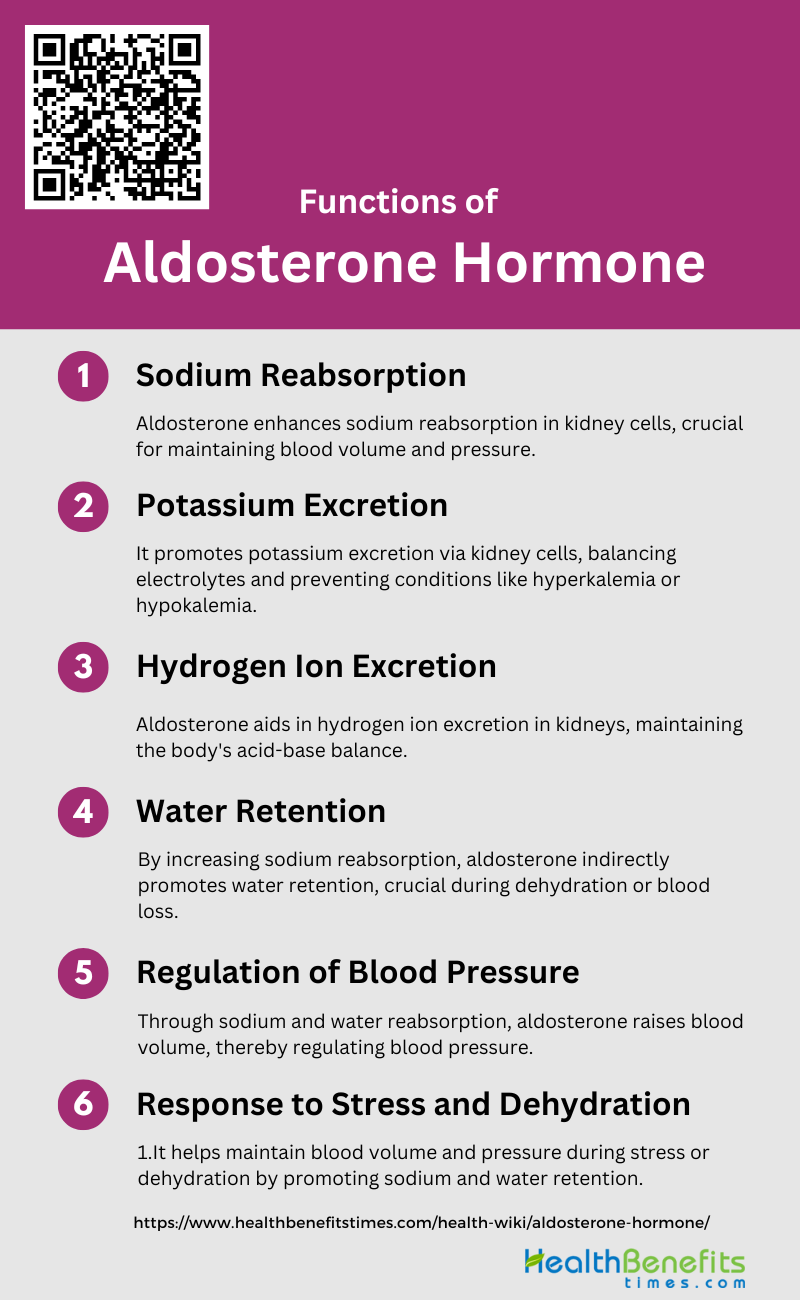
Functions of Aldosterone Hormone
Aldosterone is a hormone produced by the adrenal glands, which are located above the kidneys. It plays a crucial role in regulating the balance of electrolytes and water in the body. Here are the primary functions of aldosterone:
1. Sodium Reabsorption
It binds to mineralocorticoid receptors (MR) in epithelial cells, leading to the activation of the epithelial sodium channel (ENaC) and the sodium-potassium ATPase pump. This process increases sodium reabsorption from the tubular fluid into the bloodstream, which is essential for maintaining extracellular fluid volume and blood pressure. The regulation of sodium reabsorption by aldosterone is a key component of the renin-angiotensin-aldosterone system (RAAS), which adjusts sodium balance in response to changes in blood volume and pressure.
2. Potassium Excretion
Aldosterone significantly influences potassium excretion. When aldosterone binds to its receptors in the kidney, it enhances the activity of the sodium-potassium ATPase pump, which increases the uptake of sodium and the excretion of potassium into the urine. This process helps maintain potassium homeostasis in the body. The hormone’s ability to simultaneously promote sodium reabsorption and potassium excretion is vital for electrolyte balance and is tightly regulated to prevent imbalances that could lead to conditions such as hyperkalemia or hypokalemia.
3. Hydrogen Ion Excretion
In the distal nephron, aldosterone stimulates the secretion of hydrogen ions into the tubular fluid by increasing the activity of hydrogen ATPase pumps and hydrogen-potassium ATPase pumps. This action helps to regulate the pH of the blood by promoting the excretion of excess hydrogen ions. The hormone’s effect on hydrogen ion excretion is part of its broader role in maintaining electrolyte and acid-base homeostasis.
4. Water Retention
As sodium is reabsorbed, water follows osmotically, which helps to maintain blood volume and pressure. This process is essential for the body’s ability to conserve water during dehydration or blood loss. The hormone’s role in water retention is closely linked to its regulation of sodium balance, as the reabsorption of sodium creates an osmotic gradient that drives water reabsorption.
5. Regulation of Blood Pressure
By increasing sodium reabsorption, aldosterone raises blood volume, which in turn increases blood pressure. This mechanism is part of the RAAS, which responds to changes in blood pressure and volume to maintain homeostasis. Elevated levels of aldosterone can lead to hypertension, while insufficient aldosterone production can result in low blood pressure. The hormone’s role in blood pressure regulation is critical for cardiovascular health.
6. Response to Stress and Dehydration
Aldosterone is involved in the body’s response to stress and dehydration by promoting sodium and water retention, which helps to maintain blood volume and pressure under these conditions. During stress, the RAAS is activated, leading to increased aldosterone production. This response ensures that the body retains sufficient sodium and water to cope with the increased demands placed on it by stress or dehydration. The hormone’s ability to adjust sodium and water balance is vital for the body’s overall resilience to stress and fluid loss.
Importance of Aldosterone Hormone
Its importance extends to ensuring proper cardiovascular function and influencing kidney activity. Here are several key points that highlight the significance of aldosterone:
1. Regulates Sodium and Water Balance
Aldosterone is a critical hormone in regulating sodium and water balance in the body. It acts primarily on the kidney tubules to increase sodium reabsorption and water retention, which in turn helps maintain blood volume and pressure. This regulation is crucial for the body’s overall fluid homeostasis. The hormone achieves this by binding to mineralocorticoid receptors in the distal nephron, promoting the activity of sodium channels and transporters such as the epithelial sodium channel (ENaC) and Na,K-ATPase. This process ensures that sodium and water are reabsorbed into the bloodstream, preventing dehydration and maintaining electrolyte balance.
2. Potassium Excretion
By increasing sodium reabsorption in the kidney, aldosterone indirectly promotes the excretion of potassium ions. This is achieved through the action of the hormone on the collecting ducts of the kidney, where it enhances the activity of potassium channels, leading to increased potassium secretion into the urine. This balance between sodium reabsorption and potassium excretion is vital for maintaining proper cellular function and preventing hyperkalemia, a condition characterized by elevated potassium levels in the blood.
3. Blood Pressure Control
By increasing sodium and water reabsorption in the kidneys, it effectively increases blood volume, which in turn raises blood pressure. This mechanism is part of the renin-angiotensin-aldosterone system (RAAS), which is activated in response to low blood pressure or blood volume. Elevated levels of aldosterone can lead to hypertension, a condition characterized by persistently high blood pressure, which is a risk factor for cardiovascular diseases. Therefore, aldosterone’s role in blood pressure regulation is crucial for cardiovascular health.
4. Acid-Base Homeostasis
This hormone promotes the secretion of hydrogen ions into the urine, which helps to maintain the acid-base balance in the body. By influencing the reabsorption of bicarbonate, aldosterone ensures that the blood pH remains within a narrow, optimal range. This function is essential for various physiological processes, including enzyme activity and metabolic reactions. Disruptions in aldosterone levels can lead to acid-base imbalances, affecting overall health.
5. Electrolyte Equilibrium
By regulating the reabsorption of sodium and the excretion of potassium and magnesium in the kidneys, aldosterone ensures that electrolyte levels remain within their normal ranges. This balance is crucial for nerve function, muscle contraction, and overall cellular activity. Imbalances in electrolyte levels can lead to various health issues, including muscle weakness, cardiac arrhythmias, and neurological disturbances.
6. Cardiovascular Health
It has significant effects on cardiovascular health. Beyond its role in regulating blood pressure, aldosterone can contribute to cardiovascular inflammation and fibrosis, leading to conditions such as heart failure and vascular remodeling. Elevated aldosterone levels are associated with increased risk of cardiovascular diseases, including hypertension and congestive heart failure. The hormone’s actions on the heart and blood vessels underscore its importance in maintaining cardiovascular health and highlight the potential benefits of aldosterone antagonists in treating cardiovascular conditions.
7. Response to Stress
During stress, the renin-angiotensin-aldosterone system (RAAS) is activated, leading to increased aldosterone secretion. This helps the body retain sodium and water, ensuring adequate blood volume and pressure to cope with the stressor. Additionally, aldosterone’s effects on electrolyte balance and blood pressure regulation are crucial for maintaining homeostasis during stressful situations. Understanding aldosterone’s role in stress response can provide insights into managing stress-related health issues.
8. Fluid Homeostasis
Aldosterone is essential for fluid homeostasis, ensuring that the body’s fluid levels are balanced. By promoting sodium and water reabsorption in the kidneys, aldosterone helps maintain blood volume and pressure, which are critical for proper organ function and overall health. This hormone’s actions are particularly important in conditions of fluid loss, such as dehydration or blood loss, where it helps the body conserve water and maintain stability. Disruptions in aldosterone function can lead to fluid imbalances, affecting various physiological processes.
Disorders Associated with Aldosterone Hormone
Below is a list of disorders associated with abnormalities in aldosterone levels, highlighting the diverse impact of this hormone on bodily functions.
1. Primary Aldosteronism (Conn’s Syndrome)
Primary aldosteronism (PA), also known as Conn’s Syndrome, is characterized by the autonomous overproduction of aldosterone, leading to suppressed plasma renin activity and secondary hypertension. It is the most common endocrine cause of secondary hypertension and is associated with a high rate of cardiovascular complications. PA is often caused by bilateral adrenal hyperplasia (BAH) or aldosterone-producing adenoma (APA). Genetic mutations, particularly in ion channels and pumps, play a significant role in the pathogenesis of PA. Somatic mutations in genes such as KCNJ5, ATP1A1, ATP2B3, and CACNA1D are frequently observed in APAs, while germline mutations are implicated in familial forms of the disease.
2. Secondary Aldosteronism
Secondary aldosteronism is characterized by an overproduction of aldosterone due to an external stimulus, such as increased renin production. This condition is often a result of factors like renal artery stenosis, heart failure, or cirrhosis, which lead to increased renin-angiotensin-aldosterone system (RAAS) activity. Unlike primary aldosteronism, secondary aldosteronism involves elevated levels of both aldosterone and renin. The underlying causes of secondary aldosteronism are typically related to conditions that reduce blood flow to the kidneys, prompting the kidneys to release more renin to compensate.
3. Adrenal Hyperplasia
Adrenal hyperplasia, particularly bilateral adrenal hyperplasia (BAH), is a common cause of primary aldosteronism. BAH involves the enlargement of both adrenal glands, leading to excessive aldosterone production. This condition can be sporadic or familial, with genetic mutations playing a crucial role in its development. Somatic mutations in aldosterone-producing cell clusters and genes such as KCNJ5, CACNA1D, and ATP1A1 have been identified in BAH. These genetic insights have improved our understanding of the molecular mechanisms underlying adrenal hyperplasia and its contribution to primary aldosteronism.
4. Aldosterone-Producing Adenoma
Aldosterone-producing adenoma (APA) is a benign tumor of the adrenal gland that autonomously secretes aldosterone, leading to primary aldosteronism. APAs are often associated with somatic mutations in genes involved in ion transport and cellular signaling, such as KCNJ5, ATP1A1, ATP2B3, and CACNA1D. These mutations result in increased aldosterone production and contribute to the development of hypertension and hypokalemia. APAs are a significant cause of primary aldosteronism, and their identification is crucial for targeted treatment, often involving surgical removal of the adenoma.
5. Hypoaldosteronism (Addison’s Disease)
Hypoaldosteronism, also known as Addison’s disease, is characterized by insufficient production of aldosterone, often due to adrenal insufficiency. This condition leads to symptoms such as hypotension, hyperkalemia, and hyponatremia. Addison’s disease can result from autoimmune destruction of the adrenal cortex, infections, or genetic disorders affecting adrenal function. The lack of aldosterone disrupts the balance of sodium and potassium in the body, leading to various clinical manifestations. Treatment typically involves hormone replacement therapy to manage the deficiency and maintain electrolyte balance.
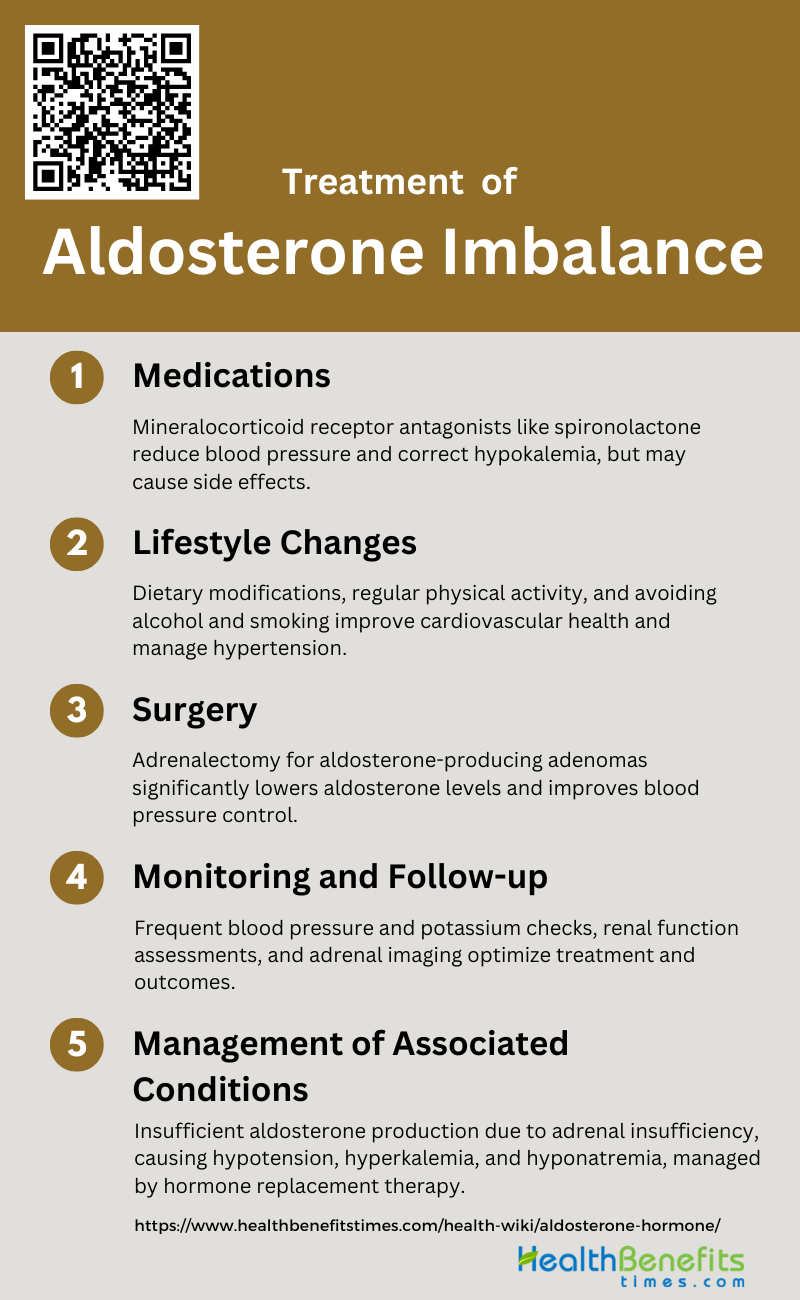
Treatment and Management of Aldosterone Imbalance
Effective treatment and management are crucial for restoring equilibrium and preventing long-term health complications. Below is a list of strategies employed in the clinical approach to address this hormonal disorder:
1. Medications
Medications play a crucial role in managing aldosterone imbalance, particularly in cases of primary aldosteronism. The primary pharmacological approach involves the use of mineralocorticoid receptor antagonists such as spironolactone and eplerenone. These medications help to block the effects of aldosterone, thereby reducing blood pressure and correcting hypokalemia. Studies have shown that these drugs are effective in controlling blood pressure and maintaining normal serum potassium levels, although they may have side effects such as hyperkalemia and gynecomastia. Additionally, combining aldosterone antagonists with other antihypertensive agents can further enhance treatment efficacy.
2. Lifestyle Changes
Lifestyle modifications are essential in managing aldosterone imbalance and its associated conditions. Dietary changes, such as reducing sodium intake, can significantly impact blood pressure control and reduce the adverse effects of aldosterone on the cardiovascular system. Regular physical activity and weight management are also recommended to improve overall cardiovascular health and reduce hypertension. Patients are advised to avoid excessive alcohol consumption and smoking, as these can exacerbate hypertension and cardiovascular risks. These lifestyle changes, when combined with medical therapy, can lead to better management of aldosterone imbalance and improved patient outcomes.
3. Surgery
Surgical intervention, specifically adrenalectomy, is often considered for patients with aldosterone-producing adenomas. This procedure involves the removal of the adrenal gland containing the adenoma, which can lead to a significant reduction in aldosterone levels and improvement in blood pressure control. Studies have shown that patients undergoing adrenalectomy often experience normalization of serum potassium levels and a reduction in the need for antihypertensive medications. However, the decision to opt for surgery versus medical management depends on various factors, including the patient’s overall health, the presence of bilateral adrenal hyperplasia, and the potential risks associated with surgery.
4. Monitoring and Follow-up
Regular monitoring and follow-up are critical components of managing aldosterone imbalance. Patients require frequent blood pressure measurements and serum potassium level checks to ensure that treatment is effective and to adjust medications as needed. Follow-up visits typically include assessments of renal function and cardiovascular health to detect any potential complications early. Imaging studies, such as adrenal CT scans, may be performed periodically to monitor the size and activity of adrenal tumors. Consistent follow-up helps in optimizing treatment plans and improving long-term outcomes for patients with aldosterone imbalance.
5. Management of Associated Conditions
Managing conditions associated with aldosterone imbalance, such as chronic kidney disease (CKD) and cardiovascular diseases, is vital for comprehensive patient care. Aldosterone antagonists have been shown to reduce proteinuria and slow the progression of CKD when used in conjunction with ACE inhibitors or ARBs. Additionally, these medications can help mitigate the risk of heart failure and other cardiovascular events by reducing fibrosis and inflammation in the heart and blood vessels. Addressing these associated conditions through a combination of pharmacological and lifestyle interventions can significantly enhance the quality of life and prognosis for patients with aldosterone imbalance.