- Vagus Nerve Stimulation (VNS) is a technique that activates the vagus nerve to influence brain and body functions.
- It helps calm the body by triggering the parasympathetic nervous system, reducing stress and improving relaxation.
- VNS is used both medically and naturally to treat conditions like epilepsy, depression, and anxiety.
 The vagus nerve is a major component of the parasympathetic nervous system, responsible for regulating crucial bodily functions like heart rate, digestion, and respiratory rate by transmitting information between the brain and various organs. Vagus Nerve Stimulation (VNS) is an innovative approach to promoting relaxation and homeostasis by electrically or manually activating this powerful nerve. When stimulated, the vagus nerve sends signals that decrease stress responses, lower heart rate, and improve emotional regulation. Research shows that non-invasive VNS techniques, including practices like chanting and yoga, can significantly reduce the physiological markers of stress and enhance parasympathetic activity. In clinical settings, VNS has been approved for treating epilepsy and depression, and ongoing research continues to explore its therapeutic potential across various conditions.
The vagus nerve is a major component of the parasympathetic nervous system, responsible for regulating crucial bodily functions like heart rate, digestion, and respiratory rate by transmitting information between the brain and various organs. Vagus Nerve Stimulation (VNS) is an innovative approach to promoting relaxation and homeostasis by electrically or manually activating this powerful nerve. When stimulated, the vagus nerve sends signals that decrease stress responses, lower heart rate, and improve emotional regulation. Research shows that non-invasive VNS techniques, including practices like chanting and yoga, can significantly reduce the physiological markers of stress and enhance parasympathetic activity. In clinical settings, VNS has been approved for treating epilepsy and depression, and ongoing research continues to explore its therapeutic potential across various conditions.
Understanding the Vagus Nerve
The vagus nerve is the longest cranial nerve in the body and plays a critical role in maintaining internal balance by relaying information between the brain and multiple organ systems, including the heart, lungs, and digestive tract. (1) Anatomically, it originates in the medulla oblongata of the brainstem and descends through the neck into the thorax and abdomen, interfacing with key systems such as the cardiovascular, respiratory, and gastrointestinal systems. This nerve is a principal component of the parasympathetic nervous system, which is responsible for the “rest and digest” functions—slowing the heart rate, stimulating digestive secretions, and promoting states of calm and recovery. (2) Its ability to regulate homeostasis makes the vagus nerve essential not only for survival but also for emotional and physiological well-being.
What Is Vagus Nerve Stimulation (VNS)?
Vagus Nerve Stimulation (VNS) refers to the application of electrical impulses to the vagus nerve to modulate its activity and thereby influence various physiological processes. There are two main types: invasive VNS, which involves surgical implantation of a stimulator device connected to the vagus nerve, and non-invasive VNS, such as transcutaneous auricular VNS, which stimulates external branches of the nerve through the skin. (3) (4) This technique is being increasingly used in clinical neurology and psychiatry due to its ability to affect brain areas involved in mood, stress, and inflammation.
Historically, VNS was first introduced as a treatment for refractory epilepsy in the late 1980s and later gained FDA approval in 1997. (5) (6) Its clinical success paved the way for broader applications, including treatment-resistant depression and even cardiovascular modulation in heart failure. (7) (8) (9) Over the years, VNS has evolved from a niche epilepsy therapy into a versatile neuromodulation platform being studied for applications in autoimmune diseases, migraine, and even long COVID. (10)
How Vagus Nerve Stimulation Calms the Body
Vagus nerve stimulation activates the body’s calming system, helping to reduce stress, lower heart rate, and improve mood. It supports relaxation by triggering the parasympathetic nervous system’s “rest and digest” response.
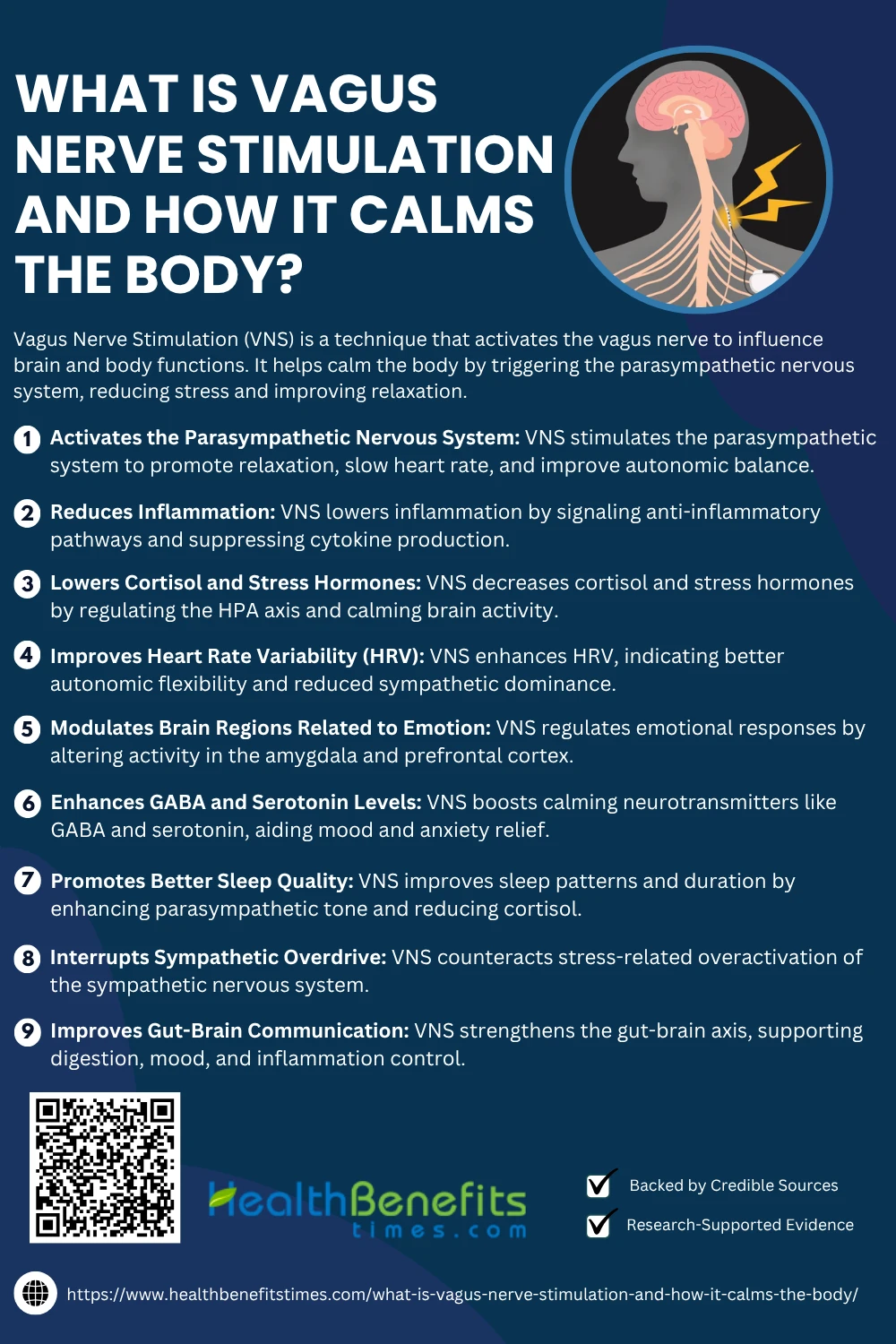 1. Activates the Parasympathetic Nervous System
1. Activates the Parasympathetic Nervous System
Vagus Nerve Stimulation (VNS) directly engages the parasympathetic nervous system, helping reduce heart rate, improve digestion, and promote relaxation. This neuromodulatory technique enhances vagal tone, facilitating the body’s shift from sympathetic “fight-or-flight” to parasympathetic “rest-and-digest” states. (11) Research shows that VNS increases baroreflex sensitivity, stabilizes blood pressure, and improves autonomic balance. It also influences the brainstem nuclei responsible for parasympathetic output, and promotes neural plasticity that strengthens parasympathetic regulation. (2) Additionally, non-invasive VNS techniques like auricular stimulation have been shown to enhance parasympathetic activity without surgery.
2. Reduces Inflammation
VNS plays a central role in reducing inflammation through the cholinergic anti-inflammatory pathway, which inhibits pro-inflammatory cytokines like TNF-α and IL-6. This modulation occurs via the vagus nerve’s efferent fibers that signal the spleen and gastrointestinal tract to suppress immune overactivation. Studies show that stimulating the vagus nerve decreases systemic inflammation in autoimmune and gastrointestinal diseases. (12) VNS also alters microglial and astrocytic activity in the brain, reducing neuro-inflammation. (13) Furthermore, researchers have found evidence that VNS may downregulate NF-κB signaling, a key inflammatory pathway. (14) Clinical trials report reduced C-reactive protein levels and other inflammatory markers in patients using VNS devices.
3. Lowers Cortisol and Stress Hormones
Vagus Nerve Stimulation (VNS) plays a key role in modulating the hypothalamic-pituitary-adrenal (HPA) axis, which governs the body’s stress response. Research confirms that VNS reduces cortisol secretion and other stress-related hormones in both clinical and experimental models. Functional MRI studies reveal VNS dampens limbic activity, contributing to reduced stress perception. Non-invasive auricular VNS has been associated with decreased salivary cortisol. It also rebalances autonomic tone, reducing sympathetic dominance. Clinical applications have shown promise in anxiety and PTSD cases by modulating endocrine stress outputs. (5)
4. Improves Heart Rate Variability (HRV)
Heart Rate Variability (HRV) reflects the balance between sympathetic and parasympathetic systems, and VNS significantly enhances HRV as a marker of improved autonomic flexibility. Transcutaneous VNS interventions have been shown to increase HRV in clinical settings. (15) This effect occurs through afferent stimulation of the vagus nerve, boosting vagal tone and baroreflex function. (16) Controlled studies also confirm improved HRV in sleep-deprived and neurodiverse populations following stimulation. (17) VNS also enhances circadian regulation of HRV in chronic conditions. (18) Furthermore, non-invasive devices like taVNS have replicated this effect across multiple populations. (19)
5. Modulates Brain Regions Related to Emotion
Vagus Nerve Stimulation (VNS) has been shown to influence emotional regulation by altering activity in key brain regions like the amygdala, prefrontal cortex, and insula. Functional neuroimaging reveals that VNS reduces hyperactivity in the amygdala, a core region involved in fear and anxiety. Simultaneously, it enhances the regulation functions of the medial prefrontal cortex. (11) Auricular stimulation also modulates default mode network activity linked to self-referential thoughts. These neuro-modulatory effects are consistent with improved mood and cognitive flexibility and have proven valuable in treating PTSD and major depressive disorder. (5)
6. Enhances GABA and Serotonin Levels
Vagus Nerve Stimulation (VNS) exerts antidepressant and anxiolytic effects in part by increasing neurotransmitters such as GABA and serotonin. Studies confirm that VNS activates brainstem nuclei like the nucleus tractus solitarius, which then stimulate serotonergic pathways in the raphe nuclei. GABA levels also rise in cortical regions post-stimulation, contributing to calmness and anti-anxiety effects. These neurotransmitter changes underpin VNS’s therapeutic use in depression, epilepsy, and generalized anxiety. (5) Auricular approaches have similarly shown neurochemical modulation with minimal invasiveness. (10)
7. Promotes Better Sleep Quality
Vagus Nerve Stimulation (VNS) significantly enhances sleep by stabilizing autonomic balance and promoting parasympathetic activity during rest. Clinical studies demonstrate that VNS improves both sleep architecture and duration in individuals with insomnia. Transcutaneous auricular stimulation has been shown to regulate circadian rhythms and increase slow-wave sleep. VNS reduces nighttime cortisol, a hormone known to disrupt sleep onset. Improved REM sleep and overall sleep efficiency were also observed in epilepsy patients receiving implanted VNS therapy. (10) Non-invasive methods like taVNS replicate these effects with fewer side effects.
8. Interrupts Sympathetic Overdrive
Vagus Nerve Stimulation (VNS) counters sympathetic overdrive by reactivating parasympathetic pathways, restoring autonomic balance. This mechanism is crucial in managing chronic stress and disorders like hypertension and anxiety. (11) Studies show VNS significantly reduces norepinephrine levels, a key marker of sympathetic activation. VNS also improves baroreflex sensitivity, enhancing blood pressure stability. Research in PTSD and panic disorder demonstrates that VNS dampens excessive sympathetic arousal. (5) Even short-term auricular stimulation can rapidly downregulate sympathetic tone.
9. Improves Gut-Brain Communication
Vagus Nerve Stimulation (VNS) enhances bidirectional communication between the gut and the brain through the gut-brain axis, significantly impacting gastrointestinal and neurological health. VNS activates afferent fibers that relay microbiota-derived signals to the brain, modulating mood and behavior. This neural relay helps regulate digestion and gut permeability. (20) Moreover, it influences enteric neurotransmission and inflammatory tone. (21) VNS also affects microbial composition and metabolite signaling pathways that impact cognition and emotion. (22) These mechanisms support therapeutic applications of VNS in treating irritable bowel syndrome and inflammatory bowel diseases. (23)
Medical Applications of VNS
Vagus Nerve Stimulation (VNS) is used medically to treat conditions like epilepsy and depression. It shows promise in managing anxiety, PTSD, migraines, and inflammatory disorders through targeted nerve modulation.
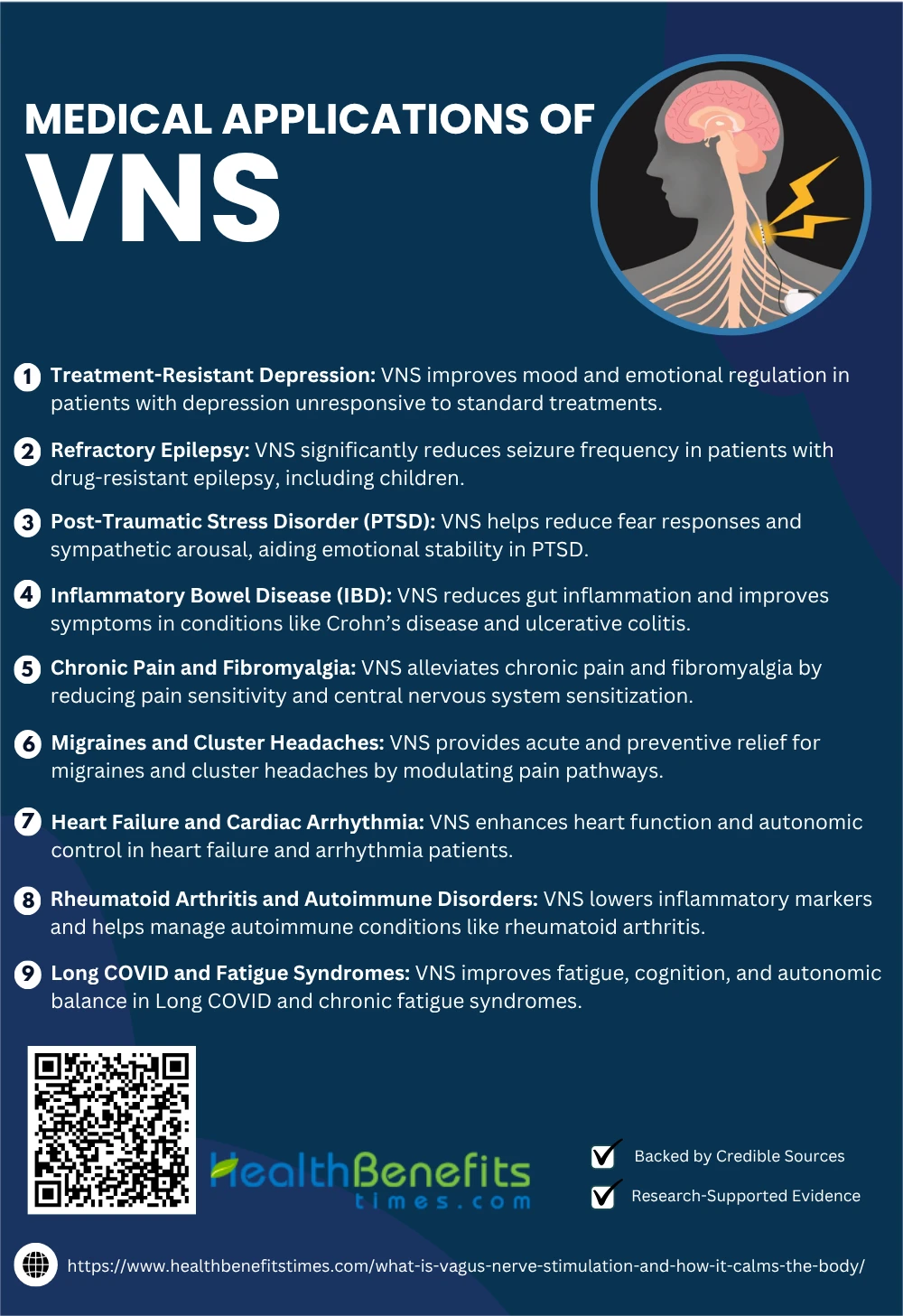 1. Treatment-Resistant Depression
1. Treatment-Resistant Depression
Vagus nerve stimulation (VNS) has shown promise for individuals with treatment-resistant depression (TRD), where conventional therapies fail. Studies indicate that VNS modulates mood-related brain circuits, improving symptoms in chronic depression. Long-term benefits are reported, especially when combined with pharmacotherapy. Meta-analyses confirm its efficacy in TRD populations, while safety and tolerability remain favorable. (24) (25)
2. Refractory Epilepsy
Vagus nerve stimulation (VNS) is a well-established adjunctive therapy for refractory epilepsy, significantly reducing seizure frequency. A comprehensive study confirmed its effectiveness in super-refractory status epilepticus cases. (26) Meta-analyses report over 50% seizure reduction in many patients. (27) Another clinical review supports its long-term benefits in pediatric epilepsy. (28) Additionally, physiological studies show VNS improves autonomic regulation during seizures. (29)
3. Post-Traumatic Stress Disorder (PTSD)
Vagus nerve stimulation (VNS) has shown therapeutic effects in post-traumatic stress disorder (PTSD) by modulating emotional reactivity and autonomic dysfunction. Studies reveal that VNS dampens hyperactive amygdala circuits involved in fear responses. It also restores vagal tone, reducing sympathetic arousal in PTSD patients. (5) Pilot trials report improved emotion regulation and sleep. Non-invasive taVNS has replicated these benefits.
4. Inflammatory Bowel Disease (IBD)
Vagus nerve stimulation (VNS) effectively reduces inflammation in inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis. Through the cholinergic anti-inflammatory pathway, VNS inhibits cytokine release and gut inflammation. Clinical studies show symptom relief and mucosal healing in IBD patients using VNS devices. (20) VNS also improves gut motility and permeability. (21) Emerging findings support microbiota modulation as another mechanism. (22)
5. Chronic Pain and Fibromyalgia
Vagus nerve stimulation (VNS) demonstrates therapeutic promise in managing chronic pain and fibromyalgia by modulating pain signaling pathways and reducing central sensitization. A 2025 review in Brain Sciences highlighted VNS’s efficacy in reducing fibromyalgia-related pain behaviors. Similarly, a randomized trial in Springer reported notable pain reduction in knee osteoarthritis. (30) Moreover, Elsevier’s review supports VNS’s broad applicability in pain conditions, as echoed by AIRR researchers. (31) (32)
6. Migraines and Cluster Headaches
Vagus nerve stimulation (VNS) is increasingly recognized for alleviating migraines and cluster headaches through neuromodulation of trigeminovascular pathways. In a 2025 case report in Wiley, VNS notably relieved chronic cluster headaches. (33) A Springer narrative review affirmed its acute and preventive benefits. (34) The gammaCore device showed reduced intensity and frequency in real-world migraine patients. (35) Additionally, Elsevier’s overview confirmed non-invasive VNS efficacy for chronic headaches. (36)
7. Heart Failure and Cardiac Arrhythmia
Vagus nerve stimulation (VNS) improves autonomic control in heart failure by enhancing parasympathetic activity and reducing sympathetic overdrive. Studies demonstrate improved heart rate variability and ejection fraction in heart failure patients treated with VNS. (7) A recent clinical trial confirmed its safety in arrhythmia control. Zannad et al., 2015 found improved quality of life with VNS therapy. Additionally, VNS stabilizes baroreflex sensitivity.
8. Rheumatoid Arthritis and Autoimmune Disorders
Vagus nerve stimulation (VNS) shows significant potential in treating rheumatoid arthritis and other autoimmune conditions by modulating inflammatory reflexes. VNS activates the cholinergic anti-inflammatory pathway, reducing cytokines like TNF-α and IL-6. (37) A Frontiers study highlights non-invasive VNS benefits in RA. (38) Springer evidence supports its efficacy in immune modulation. (12) A 2025 Wiley review confirms its role in managing systemic inflammation. (39)
9. Long COVID and Fatigue Syndromes
Vagus nerve stimulation (VNS) has emerged as a promising therapy for Long COVID and chronic fatigue syndromes (ME/CFS) by addressing autonomic dysfunction and systemic inflammation. Studies report improved fatigue, cognition, and sleep in Long COVID patients receiving taVNS. (2) A 2024 review in Springer highlights its immunomodulatory benefits. (12) Brouillard et al., 2024 confirmed HRV improvement post-VNS. Evidence from Elsevier supports symptom relief through autonomic regulation. (40)
Natural and Non-Invasive Ways to Stimulate the Vagus Nerve
Natural methods like deep breathing, cold exposure, and humming can stimulate the vagus nerve. These simple, non-invasive techniques activate your body’s relaxation response and support mental and physical well-being.
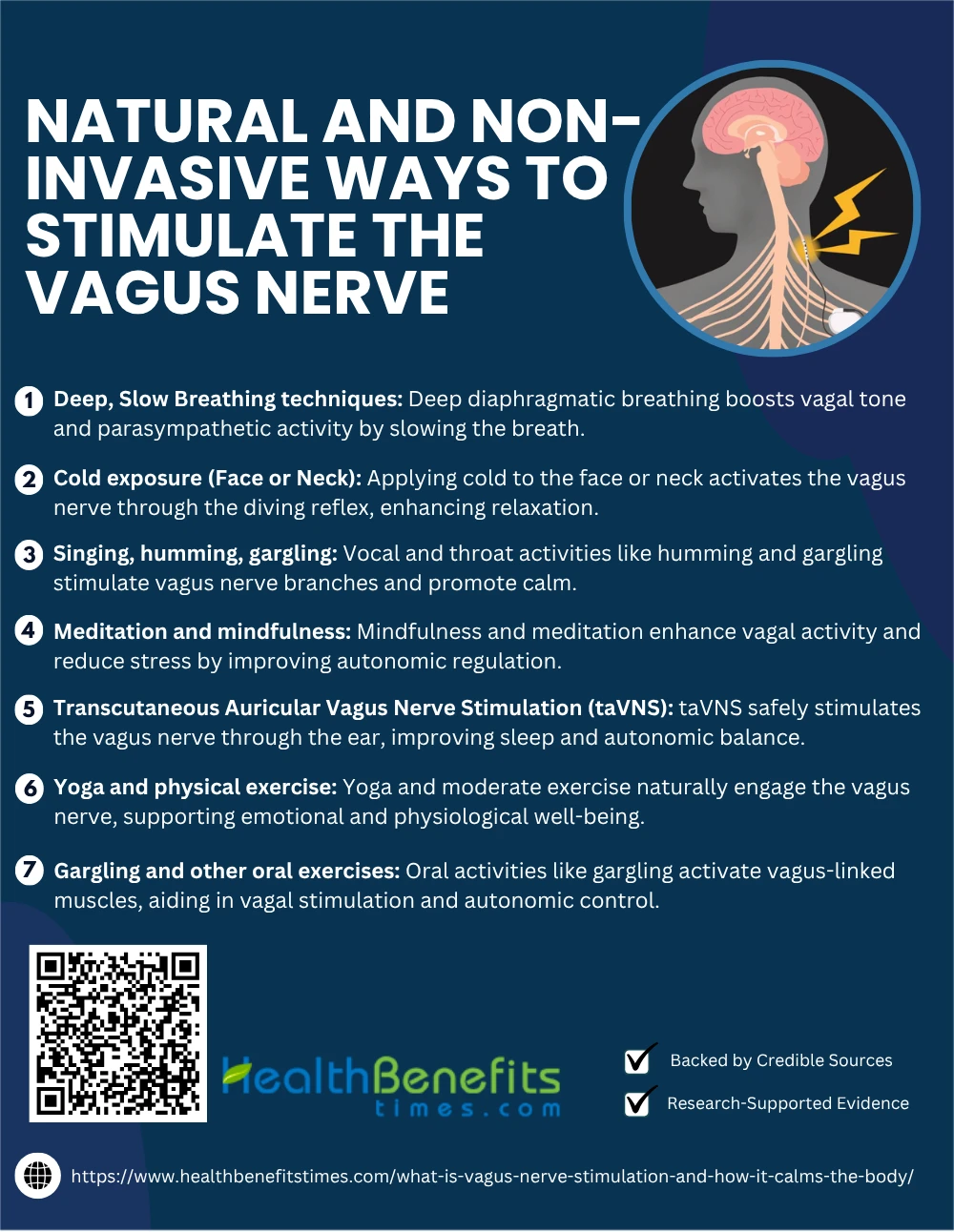 1. Deep, Slow Breathing techniques (e.g., deep diaphragmatic breathing)
1. Deep, Slow Breathing techniques (e.g., deep diaphragmatic breathing)
Deep diaphragmatic breathing is a proven, non-invasive method to stimulate the vagus nerve. By slowing the breath and engaging the diaphragm, this technique increases parasympathetic activity and enhances vagal tone. A case report confirmed that abdominal breathing significantly enhances vagal output. (41) Additional evidence shows deep breathing improves heart rate variability and reduces stress response. (42) It is widely adopted in yoga, mindfulness, and clinical therapy for its autonomic benefits.
2. Cold exposure (Face or Neck)
Cold exposure to the face or neck activates the vagus nerve through the diving reflex, reducing heart rate and enhancing parasympathetic tone. Research shows facial cold-water immersion improves vagal modulation and cardiovascular efficiency. (43) Another study demonstrated that repeated cold exposure regulates autonomic balance and improves heart rate variability. A 2024 biofeedback review also supports cold stimulus as a vagal enhancer.
3. Singing, humming, gargling
Singing, humming, and gargling are simple yet powerful techniques for naturally stimulating the vagus nerve. These vocal and throat-based activities engage the muscles at the back of the throat, activating branches of the vagus nerve and enhancing vagal tone. Research shows that chanting or humming can increase parasympathetic activity and promote relaxation. (44) Consistent gargling after brushing stimulates vagal pathways and supports stress regulation. (45) Additional findings support these methods as effective tools to boost vagal tone and improve heart rate variability. (46) These accessible practices are easy to incorporate into daily routines to foster emotional balance and physiological resilience.
4. Meditation and mindfulness
Meditation and mindfulness can significantly enhance vagal tone and parasympathetic regulation. Evidence shows mindfulness practices increase heart rate variability, a key marker of vagus nerve activity. A study by Tang et al. (2009) found improved autonomic regulation through meditation. Additionally, Goyal et al. (2014) demonstrated reduced stress markers, aligning with vagal activation mechanisms.
5. Transcutaneous Auricular Vagus Nerve Stimulation (taVNS)
Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) is a non-invasive technique that stimulates vagal afferents through the outer ear. Studies demonstrate that taVNS improves autonomic balance, reduces insomnia severity, and enhances sleep quality in clinical populations. (47) It’s considered safe and well-tolerated, with therapeutic potential across neuropsychiatric conditions. These findings support taVNS as a practical alternative to implanted VNS therapies in modulating vagal tone.
6. Yoga and physical exercise
Yoga and moderate physical exercise naturally stimulate the vagus nerve, enhancing parasympathetic activity and emotional regulation. A comparative HRV study found yoga breath techniques like Kapalbhati increased vagal tone significantly. (48) Other evidence shows that synchronized movement and respiration in yoga facilitate vagal engagement. (49) Moderate aerobic activity also supports autonomic flexibility and resilience. (50)
7. Gargling and other oral exercises
Gargling stimulates the vagus nerve via its motor fibers in the pharyngeal muscles. A case study by Cheung et al. (2010) observed oral exercises activating vagus-linked cranial nerves. (51) McPherson (2022) emphasized myofunctional therapy, including gargling, to support vagal pathways. (52) Further, Dewi et al. (2020) reported improved autonomic control in facial palsy patients using oral rehab techniques. (53)
Risks and Limitations of Vagus Nerve Stimulation
While Vagus Nerve Stimulation offers benefits, it carries risks such as voice changes, throat pain, or headaches. Limitations include inconsistent results and the need for medical supervision in certain cases.
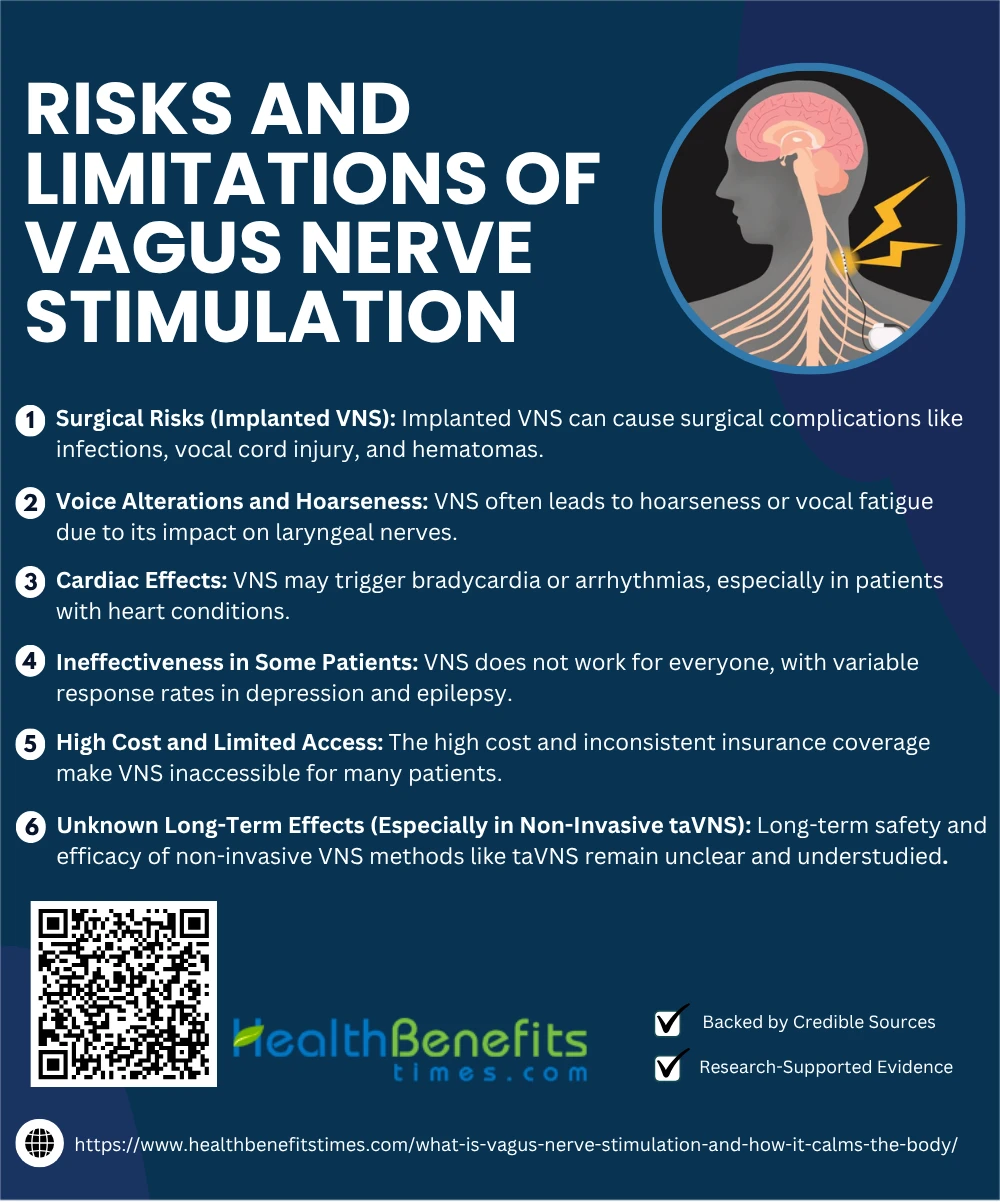 1. Surgical Risks (Implanted VNS)
1. Surgical Risks (Implanted VNS)
Implanted vagus nerve stimulation (VNS) carries inherent surgical risks, including infection, hematoma, and injury to the vocal cords. A study by Ma et al. (2024) reported complications such as vocal cord dysfunction and late-onset AV block in epilepsy patients undergoing VNS implantation. (54) Additional findings from Peterson et al. (2024) show frequent cases of hoarseness and vocal cord paresis. (55) These risks necessitate careful surgical planning and follow-up care to ensure patient safety.
2. Voice Alterations and Hoarseness
A common limitation of vagus nerve stimulation (VNS) is voice changes, including hoarseness, throat tightness, and vocal fatigue. These effects occur due to the vagus nerve’s involvement in laryngeal function. Clinical trials reported that over 60% of patients experienced voice alteration during stimulation. (5) Similar effects were noted in long-term VNS use for depression. (25) A 2025 case series also reported vocal cord paresis in VNS-treated patients. (55)
3. Cardiac Effects
Vagus nerve stimulation (VNS), especially cervical and auricular types, may induce bradycardia and arrhythmias in susceptible individuals. A study in Europace (2025) confirmed that vagally-mediated events can lead to sinus arrest or asystole in rare cases. (56) Another investigation by Zhang et al. (2025) emphasized bradycardia following right-sided VNS. (57) These risks call for pre-screening and careful device programming, particularly in patients with cardiac comorbidities. (58)
4. Ineffectiveness in Some Patients
While vagus nerve stimulation (VNS) offers benefits for many, it shows variable efficacy and is ineffective in a subset of patients. Studies in treatment-resistant depression revealed response rates between 30–50%, with delayed onset of improvement. Similar limitations were observed in epilepsy patients where seizure reduction was not universal. A 2025 review emphasized the need for biomarker-driven patient selection.
5. High Cost and Limited Access
Vagus nerve stimulation (VNS) is often cost-prohibitive, limiting accessibility for many patients. Implantation can exceed $30,000, excluding maintenance and programming costs. (24) Insurance coverage is inconsistent, particularly for off-label uses like fibromyalgia or Long COVID. Moreover, socioeconomic disparities restrict access to non-invasive taVNS devices and specialist care.
6. Unknown Long-Term Effects (Especially in Non-Invasive taVNS)
Although transcutaneous auricular vagus nerve stimulation (taVNS) is considered safe and promising, its long-term effects remain insufficiently understood. A global survey noted a wide range of user-reported side effects, emphasizing the need for clearer safety protocols. (59) Another study found that while taVNS shows analgesic benefits, long-term outcomes need evaluation. (60) Additionally, researchers caution about methodological gaps and underreporting in follow-up data. (61)
Conclusion
Vagus Nerve Stimulation (VNS) is a powerful tool that taps into the body’s natural ability to relax, heal, and restore balance. By activating the parasympathetic nervous system, VNS helps reduce stress, lower heart rate, and improve emotional well-being. Whether through medical devices or simple lifestyle practices like deep breathing or humming, stimulating the vagus nerve can support mental and physical health. While it’s not a cure-all and may not be suitable for everyone, VNS offers a promising approach for those seeking relief from chronic conditions or everyday stress. Always consult a healthcare professional before starting any new therapeutic practice.

